A Comprehensive Guide to the Symptoms of Meningitis
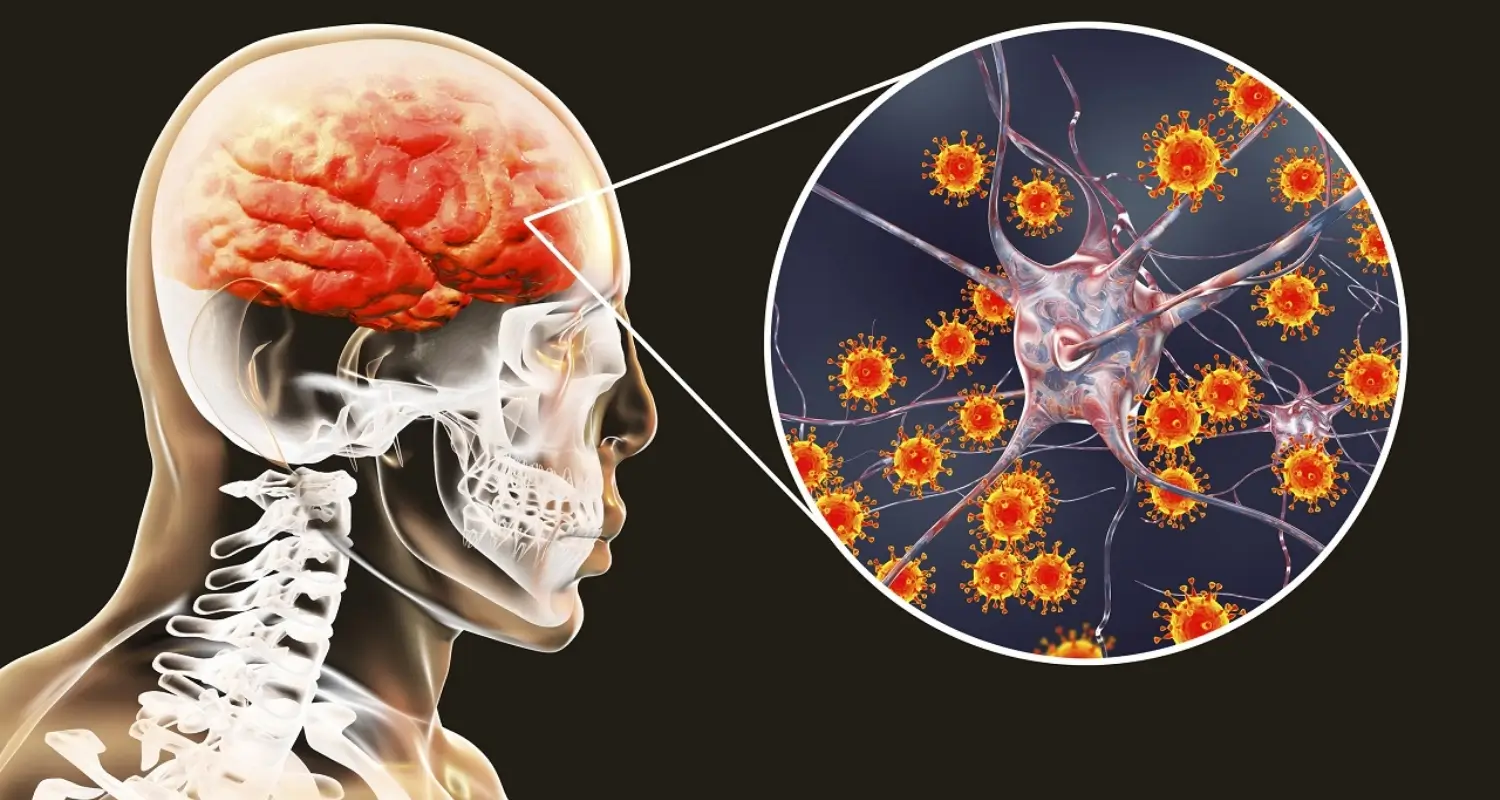
Meningitis, an infection leading to the inflammation of the brain and spinal cord’s protective layers, poses a serious health threat that requires immediate attention if the symptoms of meningitis are detected. Its causes vary, spanning from viral and bacterial to fungal and parasitic origins, making early detection critical for effective treatment. Particularly susceptible are babies, young children, teenagers, and those in young adulthood, though the risk extends across all age groups.
Identifying the symptoms of meningitis early can significantly improve outcomes, underscoring the importance of awareness and prompt medical intervention. With the brain being a primary target of inflammation in meningitis, understanding and recognizing the signs is crucial, especially during vulnerable periods such as pregnancy . This guide aims to navigate the complexities of meningitis, emphasizing the symptoms, transmission risks, and preventative measures to arm individuals with the knowledge needed to combat this condition.
Understanding Meningococcal Disease
Meningitis, a complex condition characterized by the inflammation of the membranes and fluid surrounding the brain and spinal cord, can be caused by various agents, including bacteria, viruses, fungi, and parasites. The severity and treatment of meningitis greatly depend on its cause:
- Bacterial Meningitis: Known for its acute and severe nature, bacterial meningitis demands immediate medical intervention. Common bacteria responsible include Haemophilus influenzae type b (Hib), Streptococcus pneumoniae, Neisseria meningitidis, and Listeria monocytogenes. This form of meningitis can be life-threatening if not treated promptly with antibiotics.
- Viral Meningitis: Contrasting bacterial meningitis, viral meningitis is often less severe and can resolve without specific treatment. It constitutes the majority of meningitis cases in the United States. Common viruses leading to meningitis include non-polio enteroviruses and herpesviruses.
- Other Causes: While less common, meningitis can also arise from fungal infections, particularly in individuals with weakened immune systems, or from parasitic infections like tapeworms or cerebral malaria. Non-infectious causes, such as chemical reactions, drug allergies, and certain cancers, can also lead to meningitis.
Understanding the causative agent is crucial for determining the appropriate treatment strategy and managing the condition effectively.
Symptoms of Meningitis and Early Detection
Early detection of meningitis symptoms can significantly influence the course of treatment and recovery. Recognizing these symptoms promptly in both adults and infants is critical:
- Adult Symptoms:
- Sudden high fever
- Severe headache and stiff neck
- Nausea/Vomiting
- Increased sensitivity to light (photophobia)
- Confusion or altered mental status
- Skin rash (in some cases)
- Infant Symptoms:
- High fever or hypothermia (low body temperature)
- Constant crying or irritability
- Being very sleepy, sluggish, or difficult to wake
- Poor feeding and vomiting
- Bulge in the soft spot on top of the baby’s head
- Stiffness in the body and neck
Diagnosis and Early Intervention: Diagnosis involves a comprehensive approach, including:
- Physical examination focusing on meningeal irritation and neurologic deficits.
- Lumbar puncture (spinal tap) for cerebrospinal fluid (CSF) analysis, which looks at white blood cell count, glucose, protein levels, and culture.
- Additional blood tests, stool samples, and brain imaging based on suspected causes.
Early diagnosis is paramount, especially for bacterial meningitis, to prevent severe complications such as neurological damage, seizures, or even death. For viral meningitis, symptoms generally resolve within two weeks without lasting complications, underscoring the importance of identifying the type of meningitis for appropriate management.
Transmission and Risk Factors
Understanding the transmission of meningitis and identifying risk factors are crucial steps in preventing and managing outbreaks. The bacteria responsible for meningitis primarily spread through respiratory and throat secretions, such as saliva or spit. This transmission usually requires close or prolonged contact, making individuals in the same household, roommates, or those with direct contact with a patient’s oral secretions particularly vulnerable.
Key Transmission Routes and Preventive Measures:
- Respiratory Droplets: Coughing, sneezing, or sharing utensils with an infected person can facilitate the spread.
- Preventive Actions: Good hygiene practices, including covering the nose and mouth when sneezing or coughing, can significantly reduce the risk.
Risk Factors for Meningitis:
- Age and Lifestyle: Young children, adolescents, the elderly, those living in shared residences, and individuals with incomplete vaccinations are at higher risk.
- Health Conditions: A weakened immune system, due to conditions like HIV or lupus, increases susceptibility.
- Environmental Factors: Overcrowded living conditions, such as refugee camps or student dormitories, elevate the risk.
To mitigate the spread, household contacts and others with close personal exposure to infected individuals should consider a short course of specific antibiotics. Additionally, understanding that the risk varies by the type of bacteria and organism but generally revolves around the sharing of respiratory or throat secretions, emphasizes the importance of vaccination and maintaining robust personal hygiene practices.
Treatment and Management
Treatment for meningitis varies depending on the causative organism, with bacterial and viral meningitis requiring different approaches:
Bacterial Meningitis:
- Immediate Action:
- Hospitalization is usually required.
- Antibiotics administered intravenously are the first line of treatment.
- Corticosteroids may be used to reduce inflammation.
- Supportive Care:
- Includes intravenous fluids, oxygen, and sometimes medications to control seizures.
- Preventative Measures for Close Contacts:
- Antibiotics for chemoprophylaxis, particularly against Neisseria meningitidis and Haemophilus influenzae type B.
Viral Meningitis:
- Management at Home:
- Often less severe, allowing for home treatment with rest.
- Painkillers for headaches and anti-sickness medicine for nausea.
- Hospital Care:
- In more severe cases, hospitalization for supportive care such as hydration and pain management.
General Care Guidelines:
- Diagnosis and Early Intervention:
- Critical to perform a lumbar puncture for cerebrospinal fluid analysis to identify the causative organism.
- Antibiotic therapy should begin promptly, even before the confirmation of bacterial meningitis, to mitigate the risk of severe outcomes.
- Monitoring and Long-Term Care:
- The length of hospital stay and treatment can vary, with some cases requiring several weeks.
- Close monitoring for signs of systemic complications, including hypotension, hypoxemia, and stroke, is essential.
- Seizure Control:
- Aggressive control of seizure activity is crucial for patients presenting with seizures.
Prevention and Vaccination

Vaccination stands as the cornerstone in the battle against meningitis, offering a shield against various types of this potentially deadly disease. The immunization landscape for meningitis is populated by several vaccines, each targeting different causative agents:
- Bacterial Meningitis Vaccines:
- Haemophilus influenzae type b (HiB) Vaccine: Administered to children to prevent HiB-induced meningitis.
- Pneumococcal Vaccine: Shields against pneumococcal bacteria, another common cause.
- Meningococcal Vaccine: Available in two forms, MenACWY and MenB, targeting different groups of meningococcal bacteria. The MenACWY vaccine is recommended for all preteens and teens at 11 to 12 years old with a booster dose at 16 years old, while MenB is advised for adolescents and young adults (16 through 23 years old) and younger children and adults at increased risk.
In addition to vaccination, prevention methods encompass basic hygiene practices, crucial for minimizing the spread of infections leading to meningitis. These include:
- Regular handwashing with soap and water.
- Covering the mouth and nose with a tissue or the elbow when coughing or sneezing.
- Avoiding the sharing of utensils, cups, and other personal items.
Health departments play a pivotal role in controlling meningococcal disease outbreaks by investigating each case to ensure close contacts receive appropriate prophylaxis. This targeted approach, combined with widespread vaccination efforts, forms the backbone of strategies to prevent meningitis and safeguard public health.
Conclusion
Throughout this comprehensive guide, we have navigated the complex landscape of meningitis, highlighting the critical importance of recognizing early symptoms to improve outcomes. From discussing the various causative agents, such as bacteria, viruses, fungi, and parasites, to detailing both the alarming symptoms and effective strategies for diagnosis, treatment, and prevention, this article has aimed to equip readers with essential knowledge. The guide underscores the necessity of immediate medical intervention, particularly for bacterial meningitis, and the pivotal role of vaccination in preventing the disease.
The battle against meningitis is ongoing, and awareness is our strongest weapon. Understanding the transmission risks, coupled with adopting preventive measures like good hygiene practices and vaccination, can significantly decrease the likelihood of infection. As we conclude, remember the importance of early detection and the power of informed action. Whether for oneself, loved ones, or the broader community, staying vigilant and prepared can make a crucial difference in mitigating the impact of this potentially life-threatening disease.
FAQs
What are the common symptoms one might experience if they have meningitis? The typical symptoms of meningitis can appear quite suddenly and may include a high fever, vomiting, a severe headache, a rash that doesn’t vanish when pressure is applied (such as rolling a glass over it, although a rash might not always be present), stiffness in the neck, sensitivity to bright lights, lethargy or a lack of responsiveness, and in some cases, seizures.
What are the primary indicators of meningitis that one should be aware of? Three primary signs indicating meningitis are a persistent headache, a high fever, and a stiff neck, which are caused by the inflammation associated with the condition.
What are considered the most critical symptoms of meningitis to look out for? The most alarming symptoms of meningitis, often referred to as the classic symptoms, are a high fever, severe headaches, and a pronounced neck stiffness that causes significant pain when trying to move the neck. Due to the proximity of the infection to the brain, meningitis can be extremely serious and requires immediate medical attention and treatment with appropriate antimicrobial therapy.
Which early symptoms of meningitis should prompt immediate concern? Early symptoms of meningitis that are particularly concerning and may indicate the onset of meningococcal sepsis include leg pain, cold hands and feet, and pale skin coloration. These ‘red flag’ symptoms have been observed to occur more frequently in cases of meningococcal disease than in minor, self-limiting febrile infections in children.



